Lifestyle Interventions
Adults who adhere to Guidelines which promote a healthy diet and physical activity have lower rates of cardiovascular morbidity and mortality than those who do not. In adults without overt cardiovascular risk factors counselling interventions result in improvements in health-promoting behaviors and a positive but small benefit in preventing CVD. In adults with cardiovascular risk factors, counselling interventions have a moderate benefit in preventing CVD. Most important among lifestyle interventions is the recommendation of smoking cessation. All adults should be advised to stop smoking; the benefit of smoking cessation is substantial. Dietary and exercise counselling is recommended for all individuals(i)(ii). A summary of healthy diet and impact on risk of CVD can be found in the European Society of Cardiology (ESC) 2021 guidelines.
With regards to dietary counselling, it is recommended to refer to individual national guidelines(iii)(iv).
- Leyes P, Martinez E, Talló Forga de M et al. Use of diet, nutritional supplements and exercise in HIV-infected patients receiving combination antiretroviral therapies: a systematic review. Antivir Ther.2008;13(2):149-59.
- www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/aha-diet-and-lifestyle-recommendations
- knowledge4policy.ec.europa.eu/health-promotion-knowledge-gateway/food-based-dietary-guidelines-europe-table-20_en
- 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). European Heart Journal, 42 (34): 3227–3337
Smoking cessation
Persons with HIV who smoke tobacco should be made aware of the substantial health benefits of smoking cessation which include reducing the risk of tobacco-related diseases, slowing the progression of existing tobacco-related disease, and improving life expectancy by an average of 10 years. Regularly consider the following algorithm with two major questions:
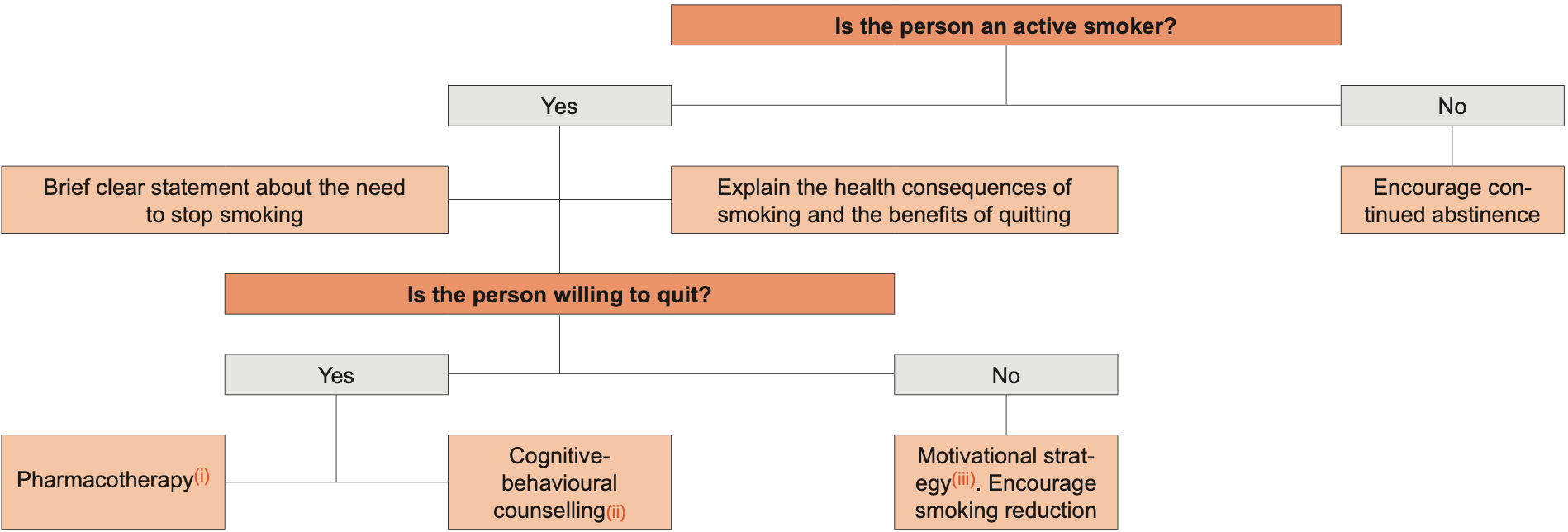
Adapted from the European Smoking Cessation Guidelines(iv) and Calvo-Sanchez M., et al, 2015(v)
- Pharmacotherapy: Nicotine replacement therapy: nicotine substitution (patch, chewing gum, spray), varenicline and bupropion are approved by the EMA. Bupropion is contraindicated with epilepsy and varenicline may induce depression. Bupropion may interact with PIs and NNRTIs, see Drug-drug Interactions between ARVs and Non-ARVs
- Cognitive-behavioral intervention: Use specific available resources
- Motivational strategy: Identify potential health risks of the smoker and to stratify both acute (e.g. exacerbations of COPD) and long-term (e.g. infertility, cancer) risks. Explain the personal benefits of stopping smoking. Identify the barriers or obstacles that might impede the success of a quit attempt. Smoking cessation interventions should be delivered repeatedly, as long as the person is not willing/ready enough to quit smoking
- ensp.network/european-smoking-cessation-guidelines-and-quality-standards/
- Calvo-Sanchez M, Martinez E. How to address smoking cessation in HIV patient HIV Med 2015; 16: 201-210 DOI:10.1111/hiv.12193
At this moment, neither EMA nor FDA approve e-cigarettes as a smoking cessation agent. In persons with HIV there is no data on long-term outcomes and it is not possible to add any more specific recommendations. EACS follows the statement issued by the CDC in 2024. www.cdc.gov/tobacco/e-cigarettes
There is inadequate evidence to determine the effect of e-cigarettes on achievement of smoking cessation as well as the harms of e-cigarettes when used as a smoking cessation tool
