Managing Older Persons with HIV
This section focuses on important issues for older persons with HIV: polypharmacy, frailty and falls that have shown to be better predictors of survival and quality of life among older people in the general population than co-morbidity alone.
Polypharmacy
Polypharmacy is defined as the concurrent use of > 5 drugs and refers to non-HIV medications given in addition to ARVs. Deprescribing or the planned and supervised process of dose reduction or stopping of medication that may cause harm, or no longer provide benefit should be incorporated in the assessment of older persons with HIV. A freely accessible resource to help deprescribe can be found at medstopper.com.
Prescribing in Older Persons with HIV
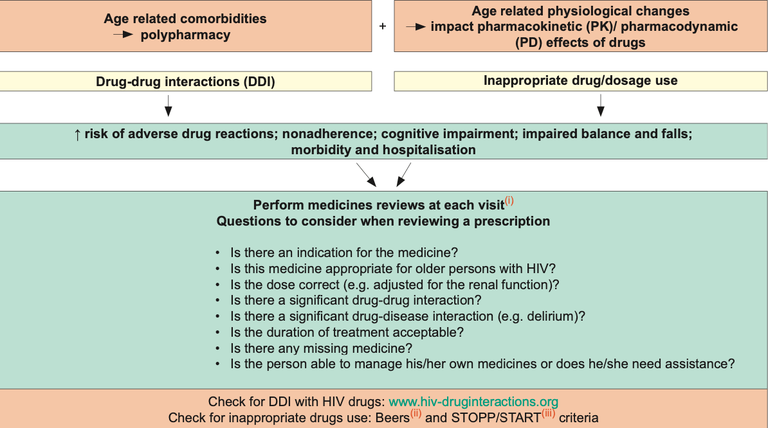
i-iii The Beers and STOPP criteria are tools established by experts in geriatric pharmacotherapy to detect and reduce the burden of inappropriate prescribing in older persons (note: these tools were established for persons > 65 years old given that PK and PD effects may be more apparent after this age cut-off). Inappropriate medicines include, for instance, those which in older persons with certain diseases can lead to drug-disease interactions, are associated with a higher risk of adverse drug reactions in older persons, medicines that predictably increase the risk of falls in the older persons or those to be avoided in case of organ dysfunction. The START criteria consist of evidence-based indicators of potential prescribing omission in older persons with specific medical conditions
Selected Top 10 Drug Classes To Avoid in Older Persons with HIV
| Drug class | Problems / alternatives |
| First generation antihistamines e.g., clemastine, diphenhydramine, doxylamine, hydroxyzine |
Strong anticholinergic properties, risk of impaired cognition, delirium, falls, peripheral anticholinergic adverse reactions (dry mouth, constipation, blurred vision, urinary retention). Alternatives: cetirizine, desloratadine, loratadine |
| Tricyclic antidepressants e.g., amitryptiline, clomipramine, doxepin, imipramine, trimipramine |
Strong anticholinergic properties, risk of impaired cognition, delirium, falls, peripheral anticholinergic adverse reactions (dry mouth, constipation, blurred vision, urinary retention). Alternatives: citalopram, escitalopram, mirtazapine, venlafaxine |
| Benzodiazepines Long and short acting benzodiazepines e.g., clonazepam, diazepam, midazolam Non-benzodiazepines hypnotics e.g., zolpidem, zopiclone |
Elderly are more sensitive to their effect, risk of falls, fractures, delirium, cognitive impairment, drug dependency. Use with caution, at the lowest dose and for a short duration. Alternatives: non-pharmacological treatment of sleep disturbance/sleep hygiene. |
| Atypical antipsychotics e.g., clozapine, olanzapine, quetiapine |
Anticholinergic adverse reactions, increased risk of stroke and mortality (all antipsychotics). Alternatives: aripiprazole, ziprasidone |
| Urological spasmolytic agents e.g., oxybutynin, solifenacin, tolterodine |
Strong anticholinergic properties, risk of impaired cognition, delirium, falls, peripheral anticholinergic adverse reactions (dry mouth, constipation, blurred vision, urinary retention). Alternatives: non-pharmacological treatment (pelvic floor exercises). |
| Stimulant laxatives e.g., senna, bisacodyl |
Long-term use may cause bowel dysfunction. Alternatives: fibres, hydration, osmotic laxatives |
| NSAIDs e.g., diclofenac, indomethacin, ketorolac, naproxen |
Avoid regular, long-term use of NSAIDs due to risk of gastrointestinal bleeding, renal failure, worsening of heart failure. Alternatives: paracetamol, weak opioids |
| Digoxin Dosage > 0.125 mg/day |
Avoid doses higher than 0.125 mg/day due to risk of toxicity. Alternatives for atrial fibrillation: beta-blockers |
| Long acting sulfonylureas e.g., glyburide, chlorpropamide |
Can cause severe prolonged hypoglycemia. Alternatives: metformin or other antidiabetic classes |
| Cold medications Most of these products contain antihistamines (e.g., diphenhydramine) and decongestants (e.g., phenylephrine, pseudoephedrine) |
First generation antihistamines can cause central and peripheral anticholinergic adverse reactions as described above. Oral decongestants can increase blood pressure. |
Legend
NSAID nonsteroidal anti-inflammatory drug
