Liver Cirrhosis: Classification, Surveillance
Child-Pugh Classification
Child-Pugh classification of the severity of cirrhosis
| Points(i) | |||
|---|---|---|---|
| 1 | 2 | 3 | |
| Total bilirubin, mg/dL (μmol/L) | < 2 (< 34) | 2-3 (34-50) | > 3 (> 50) |
| Serum albumin, g/L (μmol/L) | > 35 (> 507) | 28-35 (406-507) | < 28 (< 406) |
| INR | < 1.7 | 1.7-2.20 | > 2.20 |
| Ascites | None | Mild/Moderate (diuretic responsive) |
Severe (diuretic refractory) |
| Hepatic encephalopathy | None | Grade I-II (or suppressed with medicine) |
Grade III-IV (or refractory) |
| i | 5-6 points: | Class A |
| 7-9 points: | Class B | |
| 10-15 points: | Class C |
Surveillance Algorithm
Algorithm for surveillance for varices and primary prophylaxis
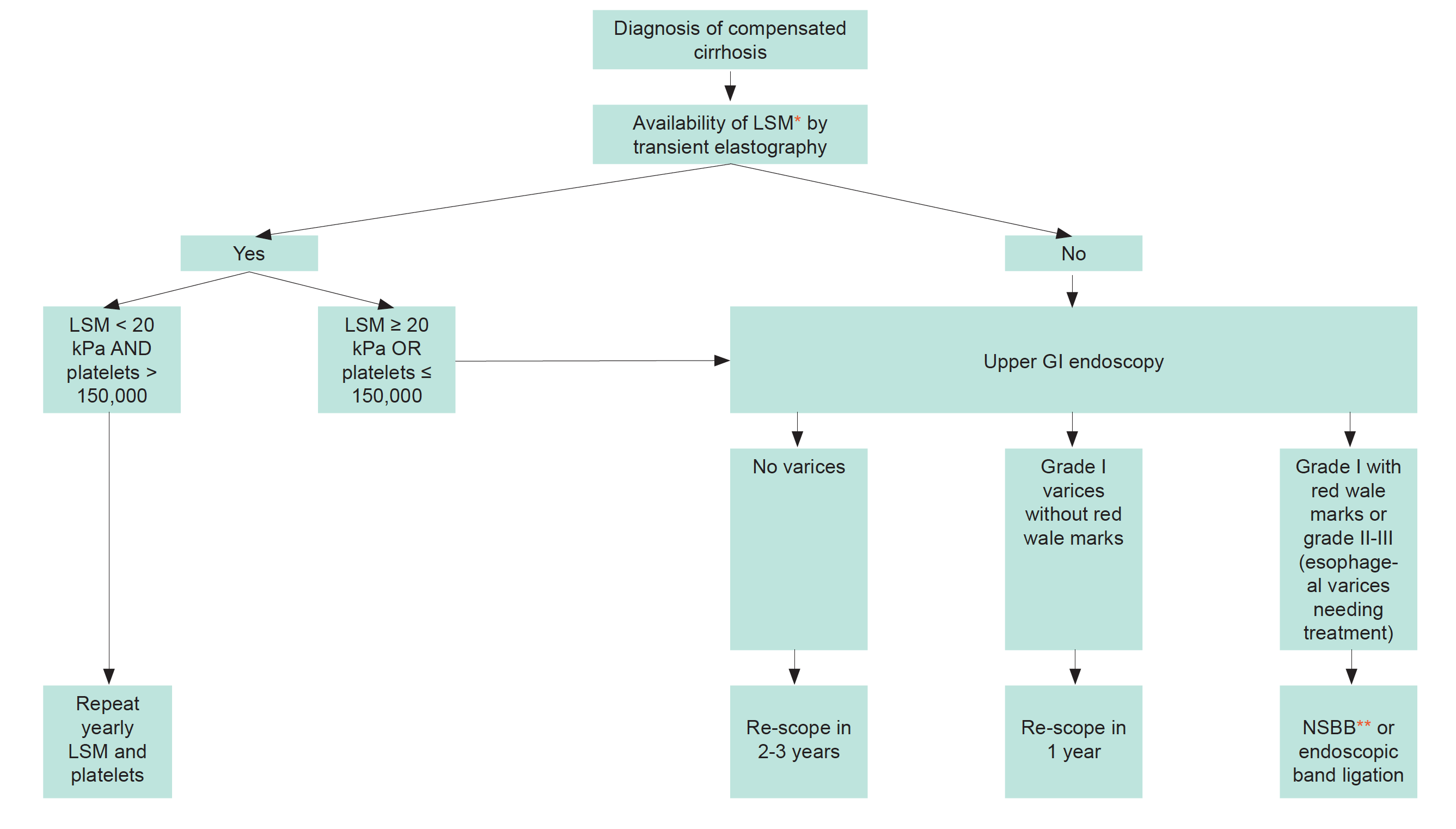
Based on Baveno VII consensus (EASL); only applicable to patients with Child-Pugh A cirrhosis. Patients with Child-Pugh B and C cirrhosis should undergo yearly gastroscopy independently of Baveno VII criteria.
*LSM, liver stiffness measurement;
**NSBB, non-selective beta-blocker: prefer carvedilol 6.25-25 mg/day
Persons with compensated cirrhosis without varices on screening endoscopy should have endoscopy repeated every 2 years with ongoing liver injury, overweight or alcohol use or every 3 years if liver injury is quiescent, e.g., after viral clearance, alcohol abstinence.
Hepatic Venous Pressure Gradient (HVPG) when available, is the gold standard and allows a direct measure of portal hypertension and prognostic stratification of persons with compensated cirrhosis.
HVPG < 6 mmHg: no portal hypertension
HVPG 6-9 mmHg: sinusoidal portal hypertension
HVPG ≥ 10 mmHg: clinically significant portal hypertension
In primary and secondary prophylaxis for variceal bleeding HVPG measurement allows to monitor efficacy of beta-blockers
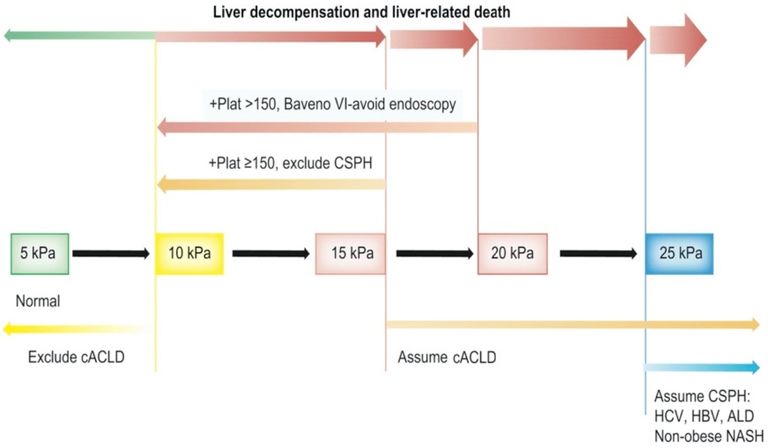
LSM by TE ≤15 kPa plus platelet count ≥150x109/L rules out clinically significant portal hypertension (sensitivity and negative predictive value >90%) in patients with compensated liver cirrhosis.
In patients with ascites and low-risk varices (small, no red signs, not Child-Pugh C), traditional NSBBs or carvedilol may be used to prevent first variceal haemorrhage. Carvedilol is the preferred NSBB in compensated cirrhosis, since it is more effective at reducing HVPG.
The Baveno VII consensus (EASL) mentions the term compensated advanced chronic liver disease (cACLD), which encompasses both advanced liver fibrosis and cirrhosis (www.journal-of-hepatology.eu/article/S0168-8278%2821%2902299-6/fulltext)
Surveillance and management for hepatocellular carcinoma should be conducted according to the EASL guidelines*.
See also Screening for complications section in the Viral Hepatitis Coinfections section.
* EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma (J Hepatol 2018, vol. 69, 182-236)
