Frailty
Frailty is defined as a clinical syndrome associated with decreased reserve, high vulnerability to stressors and associated with risk of negative health-related outcomes including mortality. Frailty should be regarded as a distinct entity to the disease or condition that may be contributing to it.
This syndrome is more prevalent than expected in persons with HIV compared to lifestyle-similar persons without HIV and may occur at an earlier age. Early identification and management of frailty is a priority since it is potentially reversible.
Screening for Frailty
Screening for frailty in persons with HIV above 50 years of age should be considered. The age cut-off was chosen as the incidence of frailty in persons with HIV has been shown to increase above this age. Evidence of benefit is still unknown. It is advocated by some experts.
Screening has to be performed using validated tools for this purpose and can be provided by any trained health staff (nurses, general practitioners, etc.). The instruments available for screening frailty are gait speed measurement, Short Physical Performance Battery (SPPB), Clinical Frailty Scale (CFS) and FRAIL Scale (FS). In the absence of a gold standard, the choice of one tool over another will depend on the available resources.
Frailty Screening Tools
Gait speed1
Description: Mark a 4-metre distance on the floor. Ask the individual to walk at usual pace from a standing start and stop the watch once they cross the 4-metre line without stopping (metres/second)
| Measure | Time | Equipment | Setting |
| Objective | Quick (< 2 min) | Stopwatch 4m space |
Clinic |
Short Physical Performance Battery (SPPB)2
Description: Test for standing balance: side by side stands, semi-tandem, and tandem plus 4-metre gait speed test plus testing the ability to rise from a chair and sit down again five times (seconds)
| Measure | Time | Equipment | Setting |
| Objective Ceiling effects |
Takes 5 min | Stopwatch 4m space A chair |
Clinic |
FRAIL Scale3
Description: Short 5-question assessment of fatigue, resistance, aerobic capacity, illnesses, and loss of weight
| Measure | Time | Equipment | Setting |
| Subjective | Quick (< 2 min) | None | Clinic Hospitalisation |
Clinical Frailty Scale (CFS)4
Description: A judgement-based frailty tool that evaluates comorbidity, function, and cognition to generate a frailty score ranging from 1 (very fit) to 9 (terminally ill)
| Measure | Time | Equipment | Setting |
| Subjective | Quick (< 2 min) | None | Hospitalisation Emergency |
1) Studenski S. JAMA. 2011;305(1):50-58. 2) Guralnik JM. J Gerontol. 1994 Mar;49(2):M85-94. 3) Morley JE, JAMDA 2013;14:392–7. 4) Rockwood K. CMAJ. 2005 Aug 30;173(5):489–495.
Algorithm Recommended for Frailty Screening
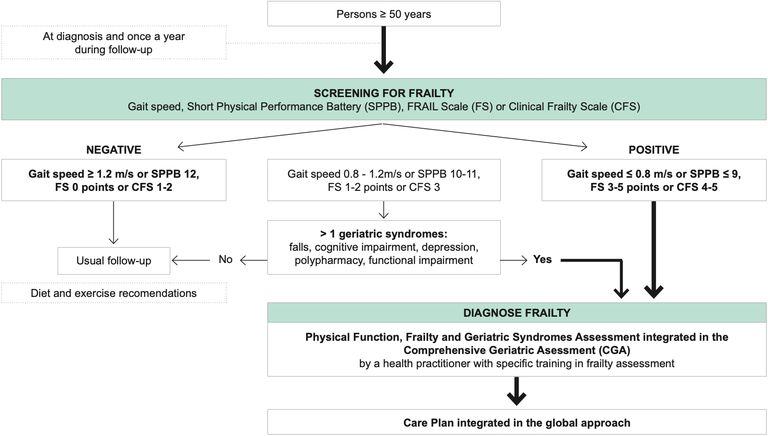
Adapted from Brañas F, Ryan P, Troya J et al. Geriatric Medicine: the geriatrician’s role. European Geriatric Medicine. 2019;10(2):259-265
Formal Frailty Assessment and Management
How to diagnose frailty
| Feature | Frailty Phenotype | Frailty Index |
| Clinical definition | Clinical syndrome based on presence of specific signs and symptoms | Based on accumulation of deficits |
| How to assess |
Assessed by five specific features: |
A frailty index is calculated based on the number of health deficits out of > 30 assessed health deficits Health variables, including signs and symptoms of disease, laboratory measures, and self-reported data Data routinely collected in medical records can be included if they characterise age-related, acquired health deficits which cover a range of physiologic systems |
| How to interpret | Categorical variables Total score of 5 items: 0 deficits = fit 1-2 deficits = pre-frail 3 + deficits = frail |
Continuous variables Index ranges from 0 to 1: ≤ 0.25 = fit 0.25 – 0.4 = frail > 0.4 = most frail |
Recommendations
| In persons with HIV who are frail: |
|
(a) Self-reported unintentional weight loss was considered present if exceeding 4.5 kg or ≥ 5% of body weight in the last year
(b) Exhaustion is present if the participant answers ‘‘occasionally’’ or ‘‘most of the time’’ to both of the following statements (questions from the Center for Epidemiologic Studies Depression Scale): During the last week, how often have you felt that 1. everything you did was an effort, or 2. you could not ‘get going’
(c) Low physical activity as considered present if the participant’s physical activity is lower than 383 kcal/week in men and 270 kcal/week in women which is equivalent to < 2.5 hours/week in men and < 2 hours/week in women using the Minnesota Leisure Time Activity Questionnaire
(d) Walk speed time, is measured by a 4-metre walking test in usual pace (one trial). A deficit is assigned according to the following gender-specific criteria
– Men: height ≤ 173 cm and speed ≤ 0.6531 m/s; height > 173 cm and speed ≤ 0.762 m/s
– Women: height ≤ 159 cm and speed ≤ 0.6531 m/s; height > 159 cm and speed ≤ 0.762 m/s
(e) Maximum grip strength can be assessed using a handheld dynamometer with the mean value of three consecutive measurements of the dominant hand (adjusted by sex and BMI quartile based on the Cardiovascular Health Study (CHS) population) as follows:
– Men: BMI ≤ 24 kg and strength < 29 kg; BMI 24.1–26 and strength < 30 kg; BMI 26.1–28 and strength < 30 kg; BMI > 28 and strength < 32 kg
– Women: BMI ≤ 23 and strength < 17 kg; BMI 23.1–26 and strength < 17.3 kg; BMI 26.1–29 and strength < 18 kg; BMI > 29 and strength < 21 kg
