Chronic Lung Disease
PWH have faster lung function decline than the background population. Age and smoking are the main risk factors, but even never-smokers have faster lung function decline than never-smokers in the background population.*
| There are 3 lifesaving interventions in COPD: |
| 1. Smoking cessation 2. Chronic oxygen when stable (non-exacerbated) resting SpO2 ≤ 88% (or PaO2 ≤ 55 mmHg) 3. Non-invasive ventilation (NIV) in individuals with persistent hypercapnia |
* Thudium RF, Ronit A, Afzal S, et al. Faster lung function decline in people living with HIV despite adequate treatment: a longitudinal matched cohort study. Thorax. 2023 Jun;78(6):535-542
Verboeket SO, Boyd A, Wit FW, et al. Changes in lung function among treated HIV-positive and HIV-negative individuals: analysis of the prospective AGEh IV cohort study. Lancet Healthy Longev. 2021 Apr;2(4):e202-e211
Pharmacological treatment of COPD(v)(vi)

Eos: eosinophils
LABA: Long Acting Beta2 Agonist
LAMA: Long Acting AntiMuscarinic
ICS: Inhaled Corticosteroid
SABA: Short Acting Beta2 Agonist
Reassess and adjust regularly according to the response to treatment in terms of symptoms and/or acute exacerbations. Adapted from GOLD 2024 (www.goldcopd.org)
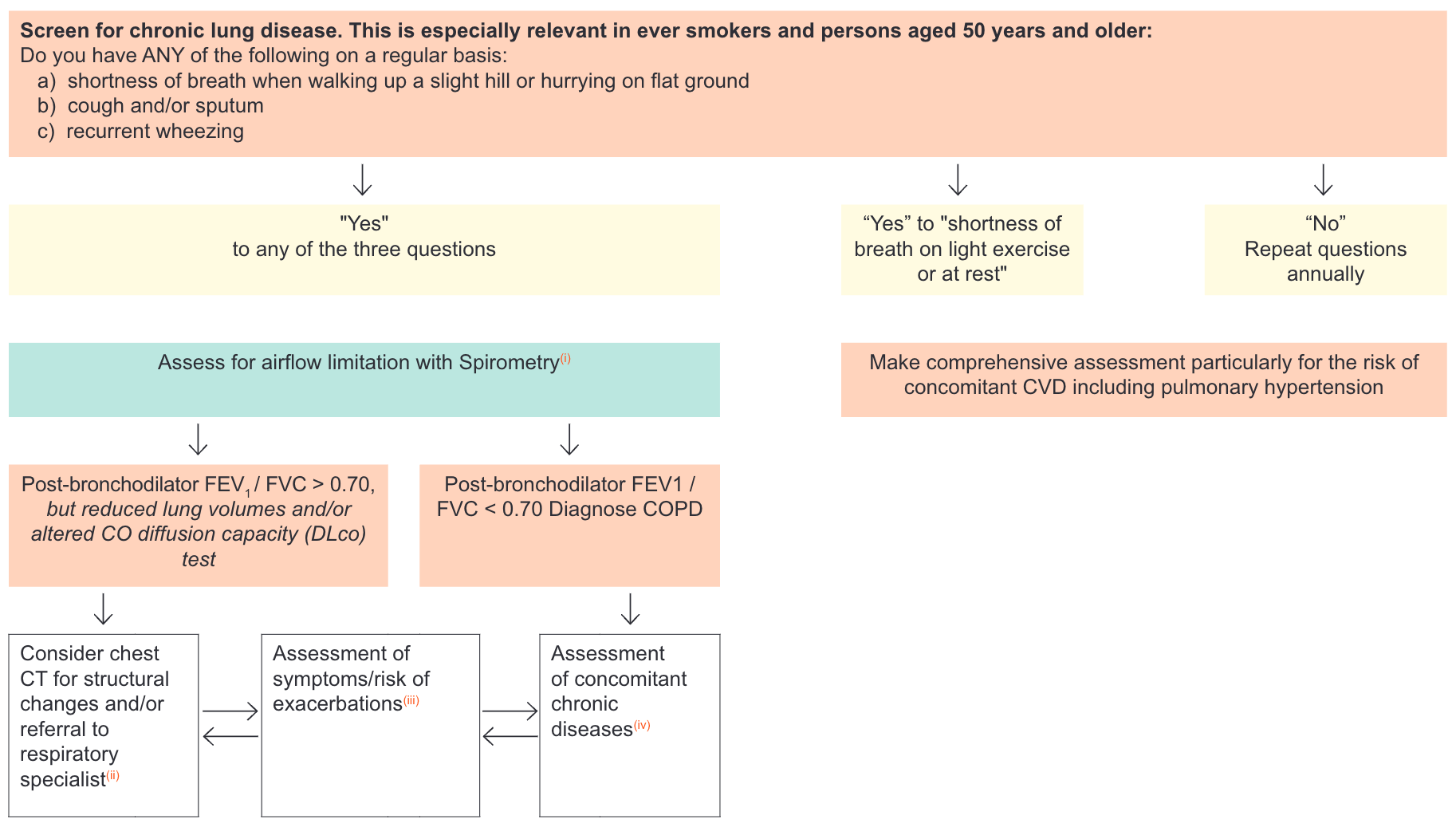
- Risk assessment for spirometry should be undertaken in the setting of COVID-19
- Based on expert opinion, also consider interstitial lung disease, CT scan may help to identify people with interstitial lung disease and lung cancer
- Assessment of either dyspnoea using mMRC, see https://www.verywellhealth.com/guidelines-for-the-mmrc-dyspnea-scale-914740 or symptoms using CAT™, see http://www.catestonline.org/ and history of exacerbations (including prior hospitalisations)
- COPD may have significant extra-pulmonary (systemic effects) including weight loss, nutritional abnormalities, frailty and skeletal mass dysfunction, and is almost invariably associated with one or more chronic comorbidities, mainly cardiovascular, respiratory and metabolic
- Each pharmacological treatment should be individualised and guided by the severity of symptoms, risk of exacerbations, adverse effects, co-morbidities, drug availability and cost, and the individual’s response, preference and ability to use various drug delivery devices. Inhaler technique needs to be assessed regularly. Long-term use of high dose ICS and/or use of oral glucocorticoids has no evidence of benefits in COPD and increase the risk of pneumonia. The addition of medium dose ICS to LABA or LAMA or LABA/LAMA is recommended in individuals with history of frequent exacerbations and/or asthma and/or eosinophilia (> 300/µL), or in individuals not adequately controlled by LAMA/LABA combinations. ICS should be avoided in subjects with eosinopenia (< 1%). Antibiotics should be used to treat acute exacerbation or in case of high CRP and purulent sputum (PCT is a more questionable biomarker). Long-term azithromycin may also be considered in non-smokers, not well controlled with maximal inhaled drug dosage
- LAMA/LABA/ICS are now available in a fixed dose combination. This drug combination improves clinical control of COPD and increases life expectancy. goldcopd.org/2024-gold-report/
With the exception of low dose beclometasone, do not use inhaled glucocorticoids with boosted ART regimens, see Drug-drug Interactions between Corticosteroids and ARVs
Influenza, SARS-CoV-2 and pneumococcal vaccination decrease rates of lower respiratory tract infections, see Immunisation in Persons with HIV
Pertussis vaccination is also suggested in people with COPD
