Prevention of Cardiovascular Disease
Principles
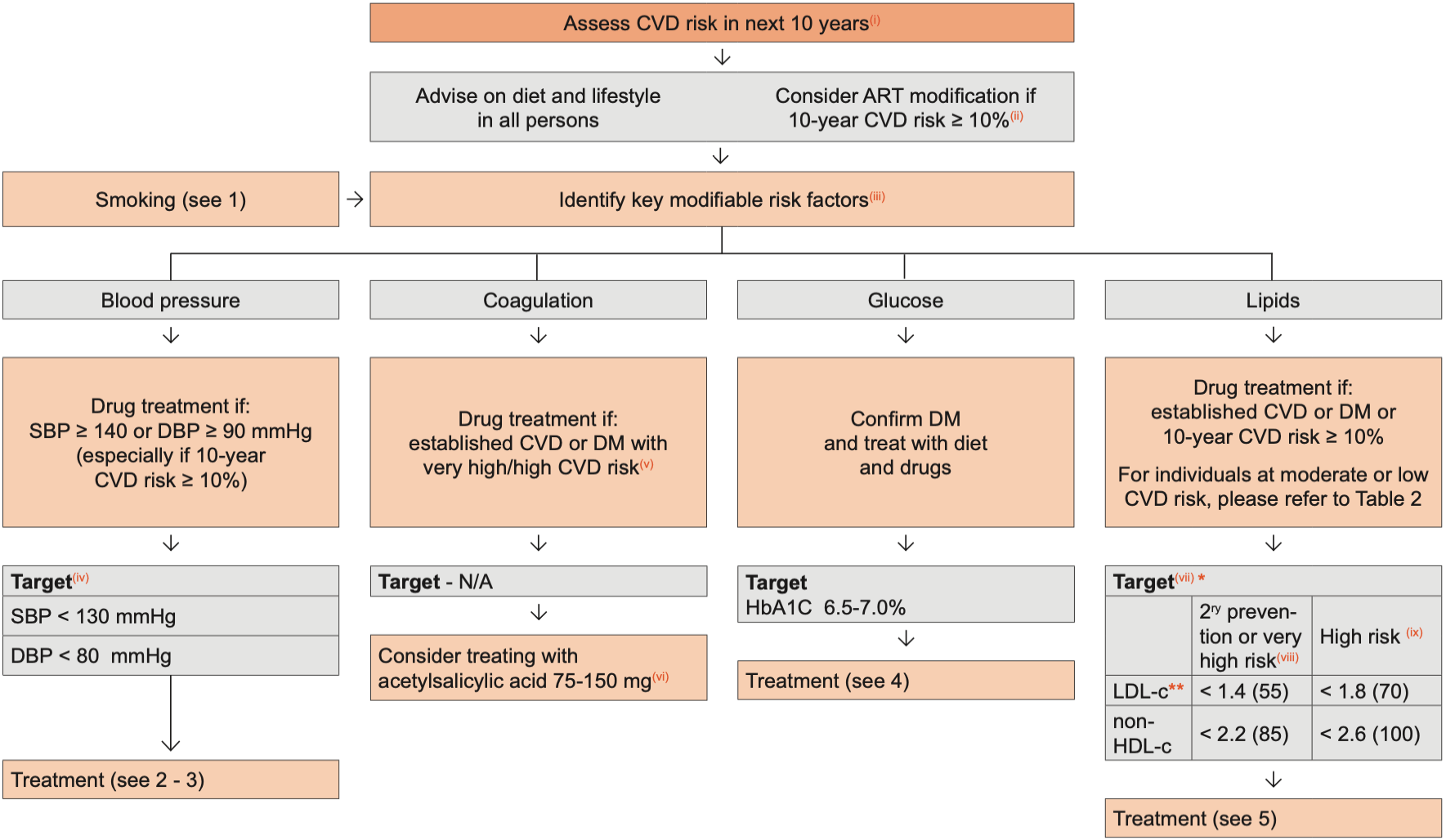
The intensity of efforts to prevent CVD depends on the underlying risk of CVD, which can be estimated(i). The preventive efforts are diverse in nature and require involvement of a relevant specialist, in particular if the risk of CVD is high and always in persons with a history of CVD
See 1: Lifestyle Interventions
See 2: Hypertension: Diagnosis, Grading and Management
See 3: Hypertension: Drug Sequencing Management
See 4: Type 2 Diabetes
See 5: Dyslipidaemia
- Use SCORE2 (40-69y) or SCORE2-OP (≥70y) as the principal tool for CVD risk estimation in primary prevention in “apparently healthy people” (subjects without atherosclerotic cardiovascular disease (ASCVD), diabetes mellitus, chronic kidney disease, or familial hypercholesterolemia). This new score includes the non-HDLc (total cholesterol - HDLc) as the lipid biomarker for CVD risk estimation and incorporates different risk score estimations depending on which country in Europe the person comes from (four European risk regions). See link below to access the CVD risk estimation calculator.
- North African and Eastern European individuals are considered at very high CVD risk
- For other ethnicities:
• Southern Asian: multiply the risk by 1.3 for people of Indian and Bangladeshi descent, and 1.7 for people of Pakistani descent.
• Other Asian: multiply the risk by 1.1.
• Black Caribbean: multiply the risk by 0.85.
• Black African and Chinese: multiply the risk by 0.7. - This assessment and the associated considerations outlined in this figure should be repeated annually in all persons receiving care, see Assessment of PLWH at Initial & Subsequent Visits, to ensure that the various interventions are initiated in a timely manner
- SCORE2 has not been validated in people with HIV and likely underestimates CVD risk estimation; HIV has been recognized as a risk enhancer for CVD
- Options for ART modification include:
(1) Replace with NNRTI or INSTI known to cause less metabolic disturbances and/or lower CVD risks, see Switch Strategies for Virologically Suppressed Persons
(2) Consider replacing ZDV or ABC with TDF or use an NRTI sparing regimen. - Observational studies suggest that smoking cessation results in about 50% less risk of IHD - and this is additive to other interventions. Of the modifiable risk factors outlined, drug treatment is reserved for certain subgroups where benefits are considered to outweigh potential harm. Of note, there is a combined benefit of various interventions in target groups identified. Per 10 mmHg reduction in systolic blood pressure, per 1 mmol/L (39 mg/dL) reduction in TC and with use of acetylsalicylic acid, each reduces risk of IHD by 20-25%; the effect is additive
- Age 65+: Target 130-139 SBP 70-79 DBP Age 18-65: 120-129 SBP 70-79 DBP Ambulatory blood pressure monitoring is recommended using home BP
- Persons with DM in the absence of clear contraindications and established CVD or other target organ damage (any proteinuria, UA/C > 3, eGFR < 30 mL/min, left ventricular hypertrophy, or retinopathy) or ≥ 3 major risk factors (age, hypertension, dyslipidemia, smoking, obesity) or early T1DM (> 20 years) or DM ≥ 10 years plus any other risk factor
- In acute settings (Post-MI, ischemic, stroke or stent insertion) dual antiplatelet therapy is recommended for up to 1 year
- Target levels are to be used as guidance and are not definitive – expressed as mmol/L with mg/dL in parenthesis. In case LDL-c cannot be measured or calculated because of high triglyceride levels, the non-HDL-c (TC minus HDL-c) target should be used. Target levels for TG are usually < 1.7 mmol/L (150 mg/dL) but the independent contribution from TG to CVD risk is uncertain
- Very high-risk persons: Documented atherosclerotic CVD (ASCVD), either clinical [ACS (MI or unstable angina), stable angina, coronary revascularization (PCI, CABG, and other arterial revascularization procedures), stroke and TIA, and peripheral arterial disease] or unequivocal on imaging [significant plaque on coronary angiography or CT scan (multivessel coronary disease with two major epicardial arteries having > 50% stenosis), or on carotid ultrasound]. DM with target organ damage, or at least three major risk factors, or early onset of T1DM of long duration (> 20 years). Severe CKD (eGFR < 30 mL/min). A very high risk calculated via SCORE2 or SCORE2-OP for fatal or non-fatal CVD. Familial hypercholesterolemia with ASCVD or with another major risk factor
- High-risk persons: Markedly elevated single risk factors, in particular TC > 8 mmol/L (> 310 mg/dL), LDL-c > 4.9 mmol/L (> 190 mg/dL), or BP ≥ 180/110 mmHg. Familial hypercholesterolemia without other major risk factors. Persons with DM without target organ damage, with DM duration ≥ 10 years or another additional risk factor. Moderate CKD (eGFR > 30 - < 60 mL/min). CVD risk estimation calculator: www.heartscore.org/en_GB/
Table 1:
SCORE2 and SCORE2-OP (ESC 2021)
|
CVD risk estimation |
< 50y |
50-69y |
≥ 70y |
|
Low / moderate |
< 2.5% |
< 5% |
< 7.5% |
|
High |
2.5 - < 7.5% |
5 - < 10% |
7.5 - < 15% |
|
Very high |
≥ 7.5% |
≥ 10% |
≥ 15% |
Adapted from the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies and with the special contribution of the European Association of Preventive Cardiology (EAPC). European Heart Journal, 42 (34): 3227–3337.
Table 2:
Proposal of statin therapy* considering the level of cardiovascular risk
| Level of CVD risk |
Very high CVD risk persons |
High CVD risk persons |
Low to moderate CVD risk persons |
|
Age > 40 y |
Recommend high-intensity statin therapy: Atorvastatin 40mg or 80mg OD Rosuvastatin 20mg or 40mg OD With LDLc target goal <55 mg/dL |
Recommend moderate or high-intensity statin therapy depending on CVD risk category: High-intensity statin**: Atorvastatin 40mg or 80mg OD Rosuvastatin 20mg or 40mg OD Moderate-intensity statin***: Pitavastatin 4mg OD Atorvastatin 20mg OD Rosuvastatin 10mg OD With LDLc target goal <70mg/dL (1.8 mmol/L) and 50% decrease from baseline LDLc |
Consider moderate-intensity statin therapy: Pitavastatin 4mg OD Atorvastatin 20mg OD Rosuvastatin 10mg OD
|
* Consider drug-drug interaction with antiretroviral medication and the required dose adjustment, where required (see “Dyslipidaemia” and “ARVs & non-ARVs” for more information). Generally, the maximum tolerated statin dose to achieve LDLc targets should be used and, if required, addition of ezetimibe should be considered if the target LDLc goal is not achieved, followed by bempedoic acid and PCSK9 inhibitors if LDLc remains above target.
** High-intensity statin is recommended in individuals with markedly elevated one or more risk factors, in particular:
- TC > 8 mmol/L (> 310 mg/dL), LDL-c > 4.9 mmol/L (> 190 mg/dL), or BP ≥ 180/110 mmHg
- Familial hypercholesterolemia without other major risk factors
- Persons with DM without target organ damage, with DM duration ≥ 10 years or another additional risk factor
- Moderate CKD (eGFR > 30 - < 60 mL/min)
- SCORE2 > 7.5% in people aged < 50 years, > 10% in people aged 50- 69 years and > 15% in people aged > 70 years
*** For individuals not considered as per the listed criteria above, moderate-intensity statin is recommended.
CVD risk estimation calculator: www.heartscore.org/en_GB/