Anti-tuberculosis Drugs & ARVs
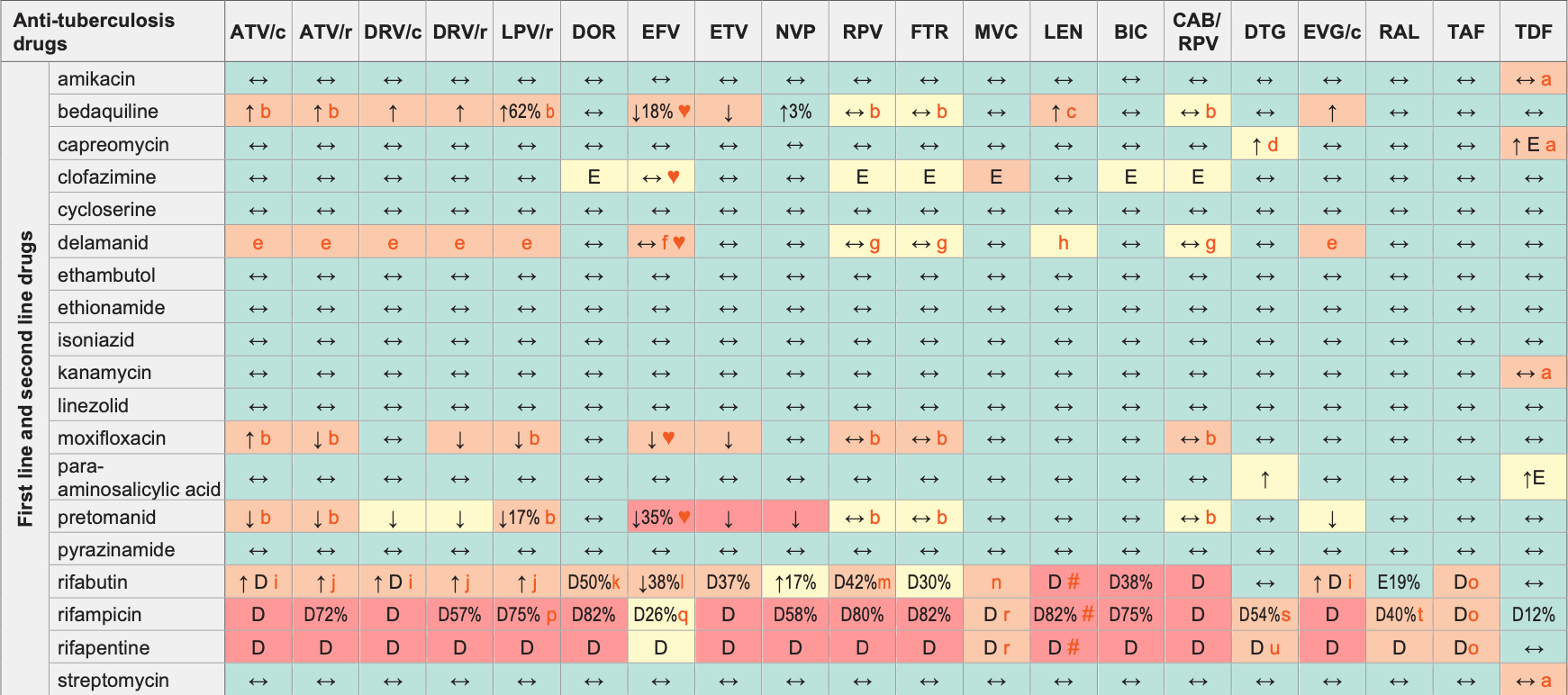
Legend
↑ Potential elevated exposure of the anti-tuberculosis drug
↓ Potential decreased exposure of the anti-tuberculosis drug
↔ No significant effect
D Potential decreased exposure of ARV drug
E Potential elevated exposure of ARV drug
Numbers refer to increased or decreased AUC as observed in drug-drug interaction studies
ATV/c:
ATV co-formulated with COBI (300/150 mg qd)
DRV/c:
DRV co-formulated with COBI (800/150 mg qd)
CAB/RPV:
CAB and RPV im long acting injections
Interactions with ABC, FTC, 3TC, ZDV
ABC:
Potentially moderately increased ABC exposure with rifampicin but no a priori dose adjustment required
FTC:
Exposure of FTC and/or capreomycin or para-aminosalicylic acid may increase when co-administered. Monitor renal function as appropriate
3TC:
Exposure of 3TC and/or capreomycin or para-aminosalicylic acid may increase when co-administered. Monitor renal function as appropriate
ZDV:
Rifampicin decreased ZDV AUC by 47%. Co-administration is not recommended in ZDV’s European label, but the US label says routine dose modification is not warranted
Interactions with cabotegravir (oral)
Decreased CAB exposure with rifampicin (59%) and rifapentine;
these drugs should not be co-administered
Interactions with ibalizumab
None
Comments
- Co-administration should be avoided due to the risk of additive tubular toxicity, but if such use is unavoidable, closely monitor renal function.
- Both drugs can potentially prolong the QT interval, ECG monitoring recommended.
- Systemic use for >14 consecutive days should be avoided. If co-administration is necessary, clinical monitoring including frequent ECG assessment and monitoring of transaminases is recommended.
- Aminoglycosides are nephrotoxic (risk is dose and treatment duration related). Renal function should be monitored as clinically appropriate and the dosage of the ARV adjusted accordingly.
- Co-administration is expected to increase concentrations of DM-6705, a delamanid metabolite which is associated with QT prolongation. Frequent ECG monitoring is recommended.
- A higher rate of neuropsychiatric adverse effects (e.g., euphoric mood and abnormal dreams) was observed with delamanid plus EFV compared to either drug alone.
- RPV, FTR and DM-6705 (a delamanid metabolite) can potentially prolong the QT interval, ECG monitoring recommended.
- Co-administration is expected to increase concentrations of DM-6705, a delamanid metabolite which is associated with QT prolongation, although to a limited extent that is not expected to increase the risk of QT prolongation.
- Reduce rifabutin to 150 mg 3 times per week.
- Reduce rifabutin to 150 mg qd. Monitoring for rifabutin-related toxicities (i.e., uveitis or neutropenia) is advised with daily administration of rifabutin.
- The product label for DOR recommends to increase DOR dosage to 100 mg bid when co-administered with rifabutin. DOR should be kept at 100 mg bid for at least another 2 weeks following cessation of rifabutin due to the persisting inducing effect upon discontinuation of a moderate/ strong inducer.
- Increase rifabutin to 450 mg qd.
- The RPV dose should be increased to 50 mg qd during co-administration (and decreased to 25 mg qd when rifabutin is stopped). Note, it is recommended to maintain RPV 50 mg qd for at least another 2 weeks following cessation of rifabutin due to the persisting inducing effect upon discontinuation of a moderate/strong inducer.
- Increase MVC to 600 mg bid in the absence of a PI. Give MVC 150 mg bid with a PI.
- Rifamycins decrease TAF exposure when given 25 mg. However, the intracellular tenofovir diphosphate (active entity) concentrations are likely to be higher than those observed with TDF even without rifampicin suggesting that usage of TAF 25 mg qd may be acceptable.
- If no other option use RTV 400 mg bid or double dose LPV/r.
- Efavirenz should be used at 600 mg qd in presence of rifampicin (in absence of rifampicin, efavirenz can be used at 400 mg qd or 600 mg qd).
- Give MVC 600 mg bid.
- A dose adjustment of DTG to 50 mg bid is recommended in treatment-naïve or INSTI-naïve persons. This dose adjustment should be maintained for 2 weeks after stopping rifampicin as the inducing effect persists after discontinuation of a strong inducer. Alternatives to rifampicin should be used where possible for INSTI-experienced persons with certain INSTI-associated resistance substitutions or clinically suspected INSTI resistance.
- RAL 400 or 800 mg bid.
- Based on DTG interactions studies with rifabutin and rifampicin, consider administering DTG at 50 mg bid in the presence of rifapentine. This dose adjustment should be maintained for 2 weeks after stopping rifapentine as the inducing effect persists after discontinuation of a strong inducer.
♥ EFV prolonged the QT interval above the regulatory threshold of concern in homozygous carriers of the CYP2B6*6/*6 allele (516T variant). Coadministration with a drug with a known risk of TdP is contraindicated in the EFV European label.
# At least a 2-week (moderate inducers) or 4-week (strong inducers) cessation period is recommended prior to initiation of LEN due to the persisting inducing effect after discontinuation of an inducer.
Further Information
For additional drug-drug interactions and for more detailed pharmacokinetic interaction data and dosage adjustments, please refer to: http://www.hiv-druginteractions.org (University of Liverpool)
